
Recently, the research results from the research project, How does Individualized Prevention Strategy Program Involving Family Members Affect Older Patients Who Undergo Noncardiac Surgical Treatment, have been published in JAMA Internal Medicine (IF=20.768), a well-known international medical journal, in the form of original research article. It proposed an individualized prevention strategy for postoperative delirium in older adults, which better tailored to the national conditions of China. Wang Yanyan, a Postdoctoral Fellow, from the Center of Gerontology and Geriatrics, WCH, is the first author, and Prof. Yue Jirong is the corresponding author, and West China Hospital is the first institute of the authors.
The randomized clinical trial (RCT) was primarily led by the Multidisciplinary Team (MDT) from the Center of Gerontology and Geriatrics of WCH, with the classic examplar of the original Hospital Elder Life Program (HELP), created by Prof. Sharon K. Inouye from the Aging Brain Center of Harvard University. We innovatively developed a family involved, individualized HELP, called t-HELP, tailoring to the cultural characteristics of care for older people and the existing resources of hospital systems in China.
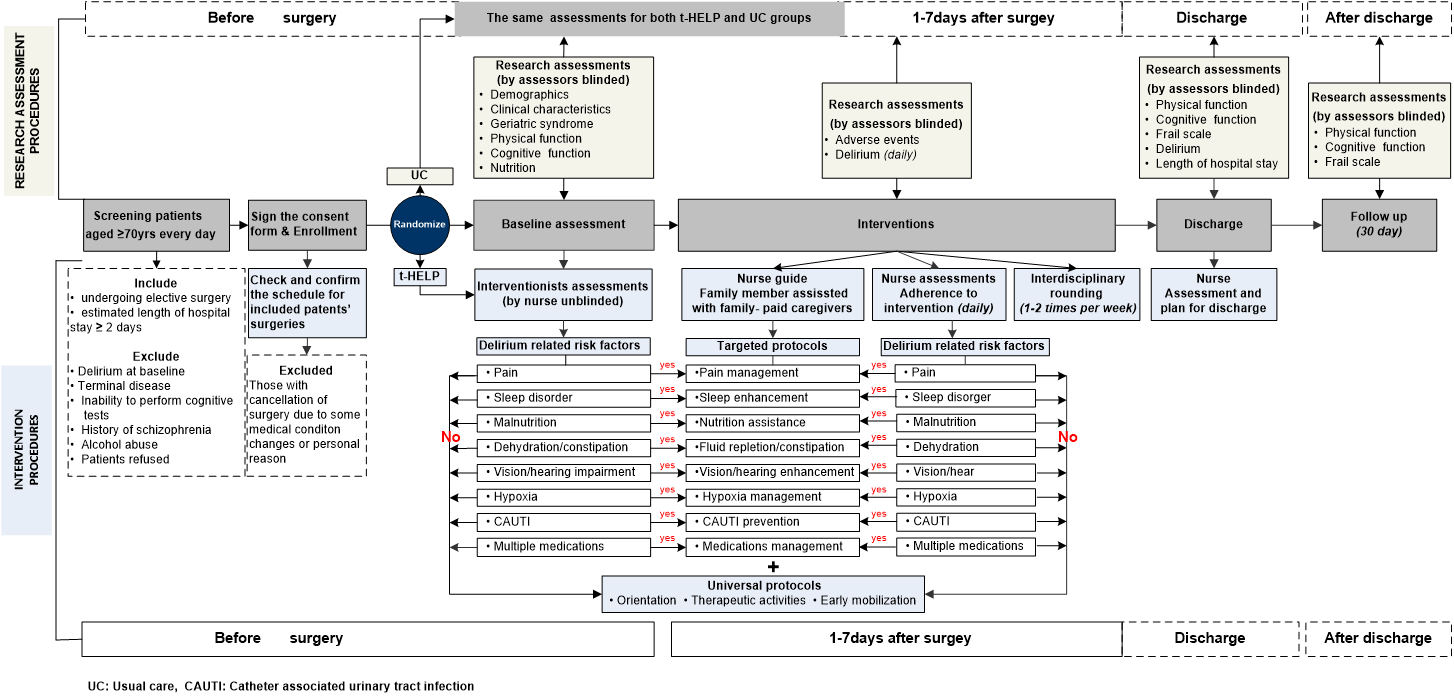
Figure 1 t-HELP research technology scheme
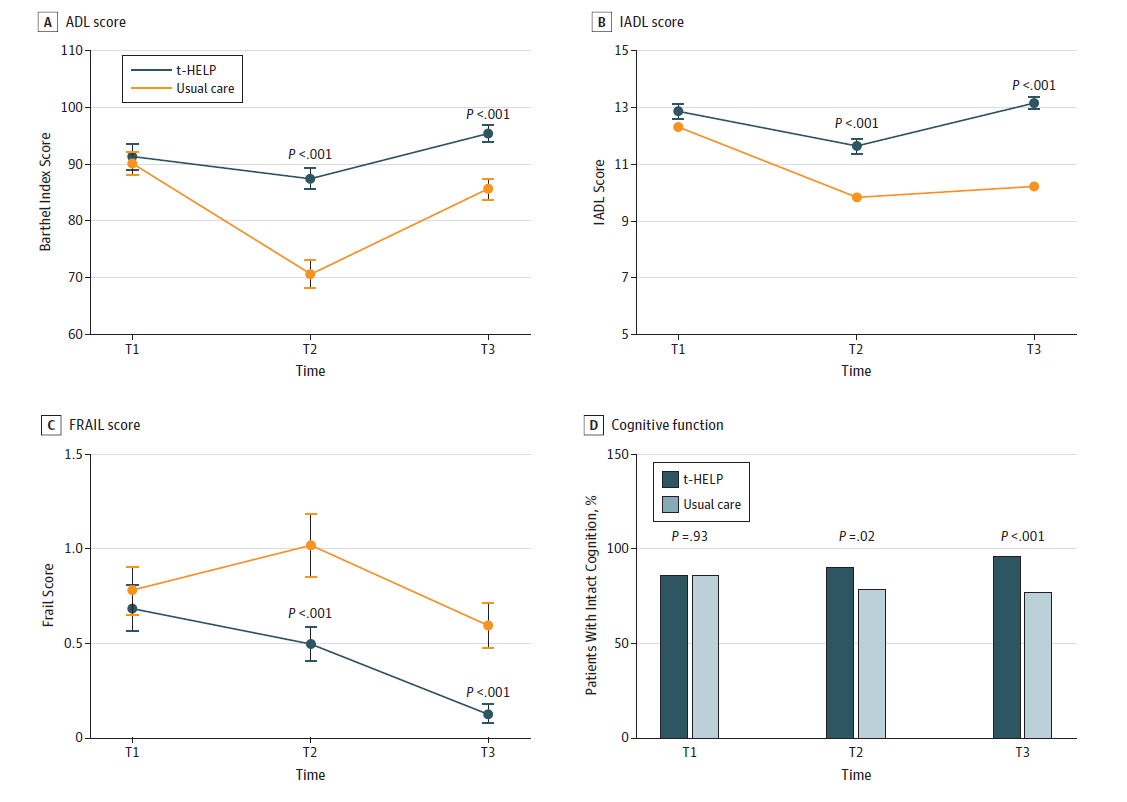
Figure 2 Longitudinal changes in physical function and cognitive function in two groups of patients from baseline to 30 days after discharge
t-HELP has customized an individualized “Menu of Prevention Strategies” for each hospitalized older adults based on his/her individualized risk factors; while due to the lack of volunteers, their family members or nursing assistants could assist the implementation of a part of the prevention protocols (Fig. 1). The RCT has been conducted in six non-cardiac surgery units, and the results of the preliminary study were reported at the 2017 International Association for Gerontology & Geriatrics (IAGG) Annual Meeting, and received positive comments from the peers.
The final results showed that the incidence rate of postoperative delirium in the intervention group was significantly lower than that in the control group (2.6% vs 19.4%); the longitudinal changes of physical function, frailty score and cognitive function in older adults in the intervention group were significantly better than those in the control group from hospital admission to 30 days post hospitalization (Fig. 2); and the patients in the intervention group experienced a shorter length of hospitalization compared to the control group (12.15 days vs 16.41 days).
A. The average ADL (Barthel index) of the control group was lower than the t-HELP group at the time of hospitalization and at the 30th day of discharge;
B. The average IADL of the control group was lower than the t-HELP group at the time of hospitalization and at the 30th day of discharge;
C. The average Frail Score of the control group was higher than the t-HELP group at the time of hospitalization and at the 30th day of discharge;
D. The proportion of the complete SPMSQ of the patients in the t-HELP group was higher than the control group at the time of hospitalization and at the 30th day of discharge.
The trial innovatively involved family members or nursing assistants to assist the implementation of the individualized prevention protocols, which provides the basis of evidence for the medical institutions worldwide with similar cultural background in terms of individualized prevention protocols and the preventive approaches for postoperative delirium in older adults.
JAMA Internal Medicine concurrently published an invited commentary--Including the Family in Perioperative Care of Older Adults—A Call for HELP, pointing out that hospitals in the United States may have much to learn from other cultures in which family and caregiver (hugong) engagement in patient care is the norm.
The old patients receiving care directly from their family members during the perioperative period could feel a strong sense of security in the unfamiliar hospital environment; and their trust in their family members or nursing assistants may help them more efficiently in early mobilization, reduction of anxiety, and sleep improvement. In addition, family members could take advantage of their previous knowledge of the patients to encourage them to proactively involve in their own recovery after surgery.
The link of the article: