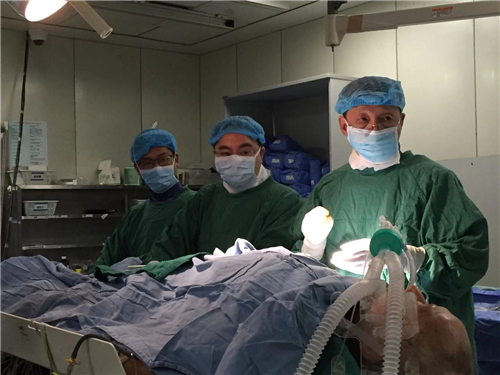
On January 16, 2020, Fang Yuan, Hu Hongde's team of pacing electrophysiology from the Department of Cardiology of WCH, successfully completed the worldwide challenging left bundle branch area pacing (LBBAP) operation via the hepatic vein with the assistance of the Department of Ultrasound and the Department of Anesthesiology. According to document retrieval, this operation demonstrated the first case of LBBAP via the hepatic vein in the world.
This patient, a 79-year-old man, underwent a conventional cardiac dual-chamber pacemaker implantation via the left subclavian vein at other hospital 9 years ago due to bradycardia and syncope. Syncope recurred 2 months ago and pacemaker battery depletion was found, so the pacemaker was replaced in a local hospital. Intraoperative test found that the threshold of the right ventricular electrode significantly increased, so the ventricle could not be effectively paced. Considering the abnormality of right ventricular electrode, the team prepared to implant a new right ventricular electrode. However, intraoperative venography found that the superior anterior chest vein was occluded, and the new electrode could not be implanted through the original vein or the contralateral vein. Therefore, the patient was transferred to WCH on January 12, 2020 from the local hospital.
The patient was old, emaciated, and thin-skinned with less muscle, so the skin may be abraded which may result in electrode damage; meanwhile, the ECG showed the third degree atrioventricular block and junctional escape rhythm, so a dual-chamber pacemaker instead of a leadless pacemaker was required. After discussion, Prof. Fang Yuan's team from the Department of Cardiology, WCH, decided to perform LBBAP via hepatic vein.
This procedure involved two of the world's leading techniques: percutaneous hepatic vein approach and left bundle branch pacing. From 2012 to 2018, the Department of Cardiology of WCH has successively implanted defibrillator (the first case in the world), dual-chamber pacemaker (the first case in China), anti-heart failure pacemaker (the first case in the world) and anti-heart failure defibrillator (the first case in the world) via hepatic vein, and has accumulated a wealth of experience. The implantation of pacing electrode via hepatic vein was thus proved to be safe and effective. Left bundle branch pacing, the world's leading pacing technology, enables to reduce the risk of cardiac growth in pacing-dependent patients with third-degree atrioventricular block. However, at present, the devices for LBBAP are mostly suitable for the "top-down" venous approach from the subclavian vein or axillary vein to the right heart. The "bottom-up" approach from the hepatic vein to the inferior vena cava and then to the right heart is difficult, and requires the physicians' dexterous hands and rich operation experience.
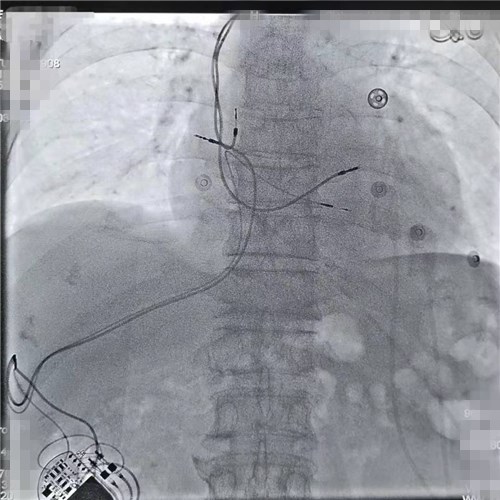
After extensive discussions and communication, Prof. Fang Yuan and Prof. Hu Hongde, with the strong support of the Department of Anesthesiology and the Department of Ultrasound, placed a temporary pacemaker through the femoral vein, and then successfully performed hepatic vein puncture. Kent-His bundle mapping was performed under the guidance of magnetic navigation and then the right ventricular electrode was screwed into the right ventricular septum 1-2cm from the connection between the distal end of Kent-His bundle and the apex of the heart through the guidance of C304 His sheath. Since the operation was conducted from bottom to top, it was very difficult for His sheath to contact the ventricle. After many attempts, Prof. Fang Yuan's team successfully implanted the right ventricular electrode in the target area. The pacing ECG showed right bundle branch block, with QRS of 130 ms and normal electrode parameters, indicating successful implantation in the left bundle branch area. Then the right atrial electrode was successfully placed, with a pacemaker pouch set in the abdomen. After the pacemaker was connected with the electrode, suture was performed and the surgery was successfully completed. On the second postoperative day, the patient was in good condition and the pacemaker functioned well.
The Fang Yuan's team from the Department of Cardiology of WCH has successfully completed all modes of transhepatic venous implantation of pacemakers. The successful combination of hepatic venous approach and world-leading LBBAP provides a new surgical approach for pacemaker-dependent patients with abnormal vascular access, and will benefit them better.